Glaucoma
Introduction to glaucoma
Glaucoma is a form of vision loss due to damage to the optic nerve which connects the eye to the brain. Damage to the optic nerve is typically due to increased pressure within the eye. The pressure pushes against the delicate optic nerve, and if excessive pressure continues over an extended period, permanent vision loss can occur.
There are several different types of glaucoma, which is usually painless and not noticed by patients until it’s too late to save their vision. Types of glaucoma have different mechanisms and, therefore, various medical (eye drops or oral medicine), laser, and surgical treatments should be considered. Dr. Reddy offers a selection of the laser and surgical options and is happy to discuss your specific case and deliver individualized care.
Types of Glaucoma
While there are different types of glaucoma, the two main categories are open-angle glaucoma and angle-closure glaucoma.
Open Angle Glaucoma
This is the most common type of glaucoma, often referred to as “the silent thief of sight” because it develops slowly and painlessly, usually with no noticeable symptoms until significant vision loss has occurred. In open-angle glaucoma, the drainage angle where the iris meets the cornea is open, but the trabecular meshwork (the drainage system of the eye) becomes less efficient over time, leading to a gradual increase in intraocular pressure (IOP). This increased pressure damages the optic nerve, resulting in peripheral vision loss that progresses slowly over time.
Angle Closure Glaucoma
Unlike open-angle glaucoma, angle-closure glaucoma is often sudden and can be considered a medical emergency. In this type of glaucoma, the drainage angle of the eye becomes blocked or closed, causing a rapid increase in IOP. This can lead to severe symptoms such as eye pain, headache, nausea, vomiting, blurred vision, halos around lights, and even sudden vision loss. Angle-closure glaucoma requires immediate medical attention to prevent permanent vision loss.
Other Types of Glaucoma
- Normal-Tension Glaucoma: In this type of glaucoma, optic nerve damage and vision loss occur despite normal intraocular pressure. The exact cause of normal-tension glaucoma is not fully understood, but it is believed that factors such as poor blood flow to the optic nerve and genetics may play a role.
- Secondary Glaucoma: This type of glaucoma develops as a result of another eye condition or medical problem, such as eye trauma, inflammation, diabetes, or the prolonged use of certain medications like corticosteroids.
- Congenital Glaucoma: Present at birth or developing in early childhood, congenital glaucoma is a rare type caused by abnormal development of the eye’s drainage system.
Diagnostics & Testing
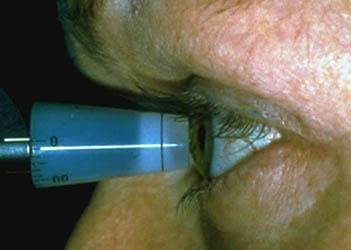
A tonometer (above) is used to check eye pressure. After applying numbing drops, the tonometer is gently pressed against the eye and its resistance is measured and recorded.

A perimetry (above) test maps the field of vision to see any pattern of changes that may indicate the early stages of glaucoma. Looking straight ahead into a white, bowl-shaped area, you’ll indicate when you’re able to detect lights as they are brought into your field of vision.

Gonioscopy (above) is used to check if the angle where the iris meets the cornea is open or closed. This helps your doctor diagnose which type of glaucoma is present – open-angle glaucoma or narrow-angle (closed) glaucoma.
Comprehensive Eye Examination
A comprehensive eye exam is the first step in diagnosing glaucoma. During this exam, your ophthalmologist will evaluate several aspects of your eye health, including:
- Visual Acuity: Testing your ability to see clearly at various distances.
- Tonometry: Measuring the pressure inside your eye (intraocular pressure or IOP). Elevated IOP is a common risk factor for glaucoma.
- Ophthalmoscopy: Examining the optic nerve at the back of the eye to look for signs of damage or cupping, which is indicative of glaucoma.
- Visual Field Testing: Assessing your peripheral vision to detect any areas of vision loss, a common symptom of glaucoma.
- Gonioscopy: Examining the drainage angle of the eye to determine if it is open or closed.
Imaging Tests
- Optical Coherence Tomography (OCT): This non-invasive imaging test provides high-resolution cross-sectional images of the retina, optic nerve, and other structures in the eye. OCT can help detect early signs of glaucoma by assessing the thickness of the retinal nerve fiber layer, which can be indicative of nerve damage.
- Gonioscopy: As mentioned earlier, this test allows the ophthalmologist to examine the drainage angle of the eye using a special lens. It helps determine whether the angle is open, narrow, or closed, which is crucial in diagnosing angle-closure glaucoma.
Visual Field Testing (Perimetry)
This test maps out your peripheral vision to detect any areas of vision loss. Visual field testing can help identify defects caused by glaucoma and monitor changes in vision over time.
Pachymetry
Measuring the thickness of the cornea (corneal pachymetry) can help assess the accuracy of intraocular pressure measurements. Thinner corneas may falsely lower IOP readings, while thicker corneas may artificially elevate them.
Regular Monitoring and Follow-Up
After the initial diagnosis, regular monitoring and follow-up appointments with your ophthalmologist are essential for managing glaucoma. Depending on the severity and progression of the disease, you may need more frequent evaluations and adjustments to your treatment plan.
Early detection and proactive management are key to preserving your vision and maintaining eye health. If you have any concerns about glaucoma or are due for an eye examination, schedule an appointment with your ophthalmologist promptly.
Treating Glaucoma
The goal of treatment is to slow down the progression of the disease and preserve your vision. The doctors at Slade and Baker Vision Center will use one of three basic types of treatment for glaucoma to lower the pressure in the eye: medicine (eye drops or oral medications), laser therapy, microsurgery, minimally invasive glaucoma surgery (MIGS).
Medicines work by slowing the production of fluid inside the eye or by improving the outflow of fluid through the drainage pathways. Some of these medications have undesirable side effects, so we will work with you to determine which treatment options control your eye pressure with the least side effects. Medicine regimens should not be stopped without talking to us first, and you should notify all your other physicians about the glaucoma medications you are taking.
For patients with narrow angle glaucoma or angle closure glaucoma, the anatomy of the front of the eye results in closure of the natural drainage pathway, which can cause high eye pressure resulting in glaucoma. In this case, options may include Laser Peripheral Iridotomy (LPI) or Clear Lens Extraction (CLE) to reduce the risk of acutely elevated eye pressure or development/progression of glaucoma. In the case of Clear Lens Extraction surgery, the new intraocular lens is significantly narrower than the natural human lens, which would allowing the drainage angle to open up and less likely to result in elevated pressure and glaucoma.
Selective Laser Trabeculoplasty (SLT)
Selective Laser Trabeculoplasty (SLT) treats the drainage canal to improve outflow and reduce eye pressure. This procedure requires only numbing eye drops and is non-surgical. The treatment is applied to the trabecular meshwork, improving the rate of drainage. SLT often reduces the need for daily medications and reduces the risk of worsening glaucoma.
Glaucoma Surgery
When medications or laser treatments fail to control glaucoma effectively, traditional incisional glaucoma surgery may be recommended by your eye doctor. Glaucoma surgery aims to lower intraocular pressure (IOP) to prevent further damage to the optic nerve and preserve vision. There are various types of glaucoma surgeries, each performed with the goal of reducing IOP.
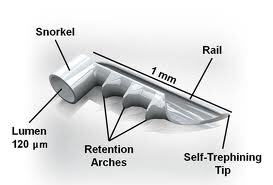
There are several minimally invasive glaucoma surgery options, including iStent, Hydrus Microstent, Canaloplasty, GATT (Gonioscopy-Assisted Transluminal Trabeculotomy), Glaucoma Drainage Implant Surgery, Traditional Filtration Surgery/Trabeculectomy.
Your doctor will discuss surgical options with you and may recommend combining glaucoma surgery with cataract surgery to improve both intraocular pressure and vision. Intraocular lens implants (IOLs) are placed during cataract surgery to improve vision, with various options available based on individual needs and preferences. Some of the advanced lens implant options that are available include Light Adjustable, Multifocal, Vivity, Toric, and Monofocal lenses.
Regardless of the treatment option chosen, regular monitoring and follow-up appointments with your ophthalmologist are essential for managing glaucoma effectively. Your healthcare provider will assess your response to treatment, monitor changes in intraocular pressure and visual field, and make any necessary adjustments to your treatment plan. It’s essential to work closely with your ophthalmologist to develop a personalized treatment plan that addresses your specific needs and preferences. With proper management and adherence to treatment, many individuals with glaucoma can maintain good vision and quality of life.

The doctors at Slade and Baker Vision have either authored or reviewed and approved this content.